The 9 Essential Components of the Mental Status Exam: The Ultimate Guide to Psychological Assessment
Have you ever wondered what mental health professionals are actually looking for when they conduct a mental health status exam? That notepad they’re scribbling on isn’t just for doodles—it’s likely documenting a structured evaluation called a mental state examination. This crucial assessment tool helps clinicians understand your psychological functioning at a specific moment in time, providing valuable insights that guide diagnosis and treatment planning.
As someone who’s both administered and received mental health status exams, I can tell you they’re much more than just a checklist. Let’s explore what mental health status exams involve, why they matter, and what you can expect if you encounter one in your mental health journey.
Table of Contents
What Is a Mental Health Status Exam?
A mental health status exam (MSE) is a structured assessment of a person’s current psychological functioning. Unlike psychological testing that might involve standardized questionnaires or lengthy evaluations, the mental health status exam captures a snapshot of your mental state during a clinical encounter.
Think of it as the psychological equivalent of a physical exam. Just as a doctor checks your heart rate and blood pressure, a mental health professional systematically observes and documents key aspects of your mental functioning. The mental health status exam provides objective data about how you’re thinking, feeling, and behaving in the moment.
The beauty of this assessment lies in its adaptability. Clinicians can conduct a brief mental health status exam during a regular therapy session or perform a more comprehensive evaluation during an initial assessment or crisis situation.
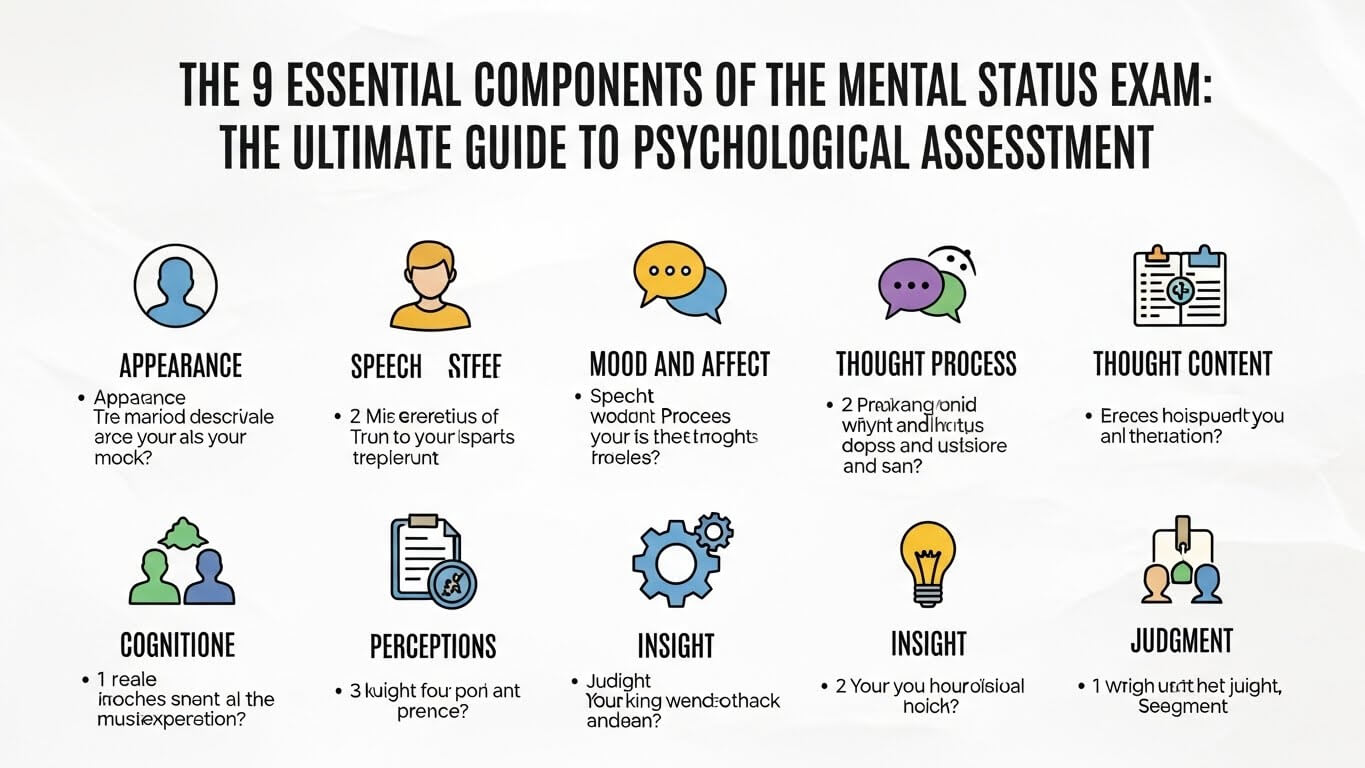
Essential Elements of the Mental Health Status Exam
A thorough mental health status exam evaluates several key domains. While different settings may emphasize certain areas over others, a comprehensive MSE typically includes:
Appearance and Behavior
The assessment begins the moment you walk into the room. The clinician observes:
- General appearance (grooming, dress, hygiene)
- Motor activity (restlessness, psychomotor agitation/retardation)
- Eye contact and facial expressions
- Unusual movements or mannerisms
- Attitude toward the examiner (cooperative, guarded, hostile)
These observations can reveal valuable information. For example, disheveled appearance might indicate depression or psychosis, while excessive movements could suggest anxiety or neurological issues.
Speech
Your manner of speaking provides important clues about your mental state:
- Rate (rapid, slow, pressured)
- Volume (loud, soft, variable)
- Quantity (verbose, limited, normal)
- Fluency and articulation
- Spontaneity and tone
Someone experiencing mania might speak rapidly with difficulty being interrupted, while a person with depression might speak slowly with long pauses.
Mood and Affect
Assessing Emotional State in Psychological Assessment
This component examines your emotional experience and expression:
- Mood: Your self-reported emotional state (“I feel sad”)
- Affect: The outward expression of emotion observed by the clinician
Clinicians note the quality (sad, anxious, irritable), range (full, restricted, blunted, flat), intensity, and appropriateness of your emotional presentation. Discrepancies between reported mood and observed affect can be particularly meaningful. For instance, describing intense sadness while smiling might suggest incongruent affect, which occurs in certain conditions.
Thought Process
This examines how you think—the form rather than the content:
- Organization and logic of thoughts
- Associations between ideas (loose, tangential, circumstantial)
- Flow and continuity
- Presence of thought blocking or racing thoughts
Disorganized thinking might indicate psychosis, while racing thoughts could suggest mania or severe anxiety.
Thought Content
Here, the focus shifts to what you’re thinking about:
- Preoccupations or obsessions
- Phobias or fears
- Suicidal or homicidal ideation
- Delusions or unusual beliefs
- Ruminations
This component is crucial for safety assessment and identifying symptoms of specific disorders like OCD or psychotic disorders.
Perceptual Disturbances
The clinician assesses for hallucinations or illusions across sensory modalities:
- Auditory (hearing voices or sounds)
- Visual (seeing things others don’t)
- Tactile (feeling sensations on/in the body)
- Olfactory/gustatory (smelling/tasting things not present)
The examiner notes the nature, content, and the person’s reaction to these experiences.
Cognition
This domain evaluates basic cognitive functions:
- Orientation (awareness of person, place, time, situation)
- Attention and concentration
- Memory (immediate, recent, remote)
- Intelligence (estimated general knowledge)
- Abstract thinking
- Judgment and insight
For a comprehensive cognitive assessment, the clinician might incorporate brief standardized tests like the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA).
Insight and Judgment
This assesses your:
- Awareness of your condition and symptoms
- Understanding of how your mental health affects your life
- Decision-making capacity
- Ability to foresee consequences of actions
Poor insight is common in certain conditions like psychosis, where someone may not recognize they’re experiencing symptoms.
The Clinical Significance of Mental Health Status Exams
Mental health status exams serve several important purposes:
- Diagnostic Clarification: The pattern of findings can help distinguish between different mental health conditions. For example, pressured speech, grandiose thoughts, and elevated mood may suggest bipolar disorder, while thought disorganization, delusions, and flat affect might point toward schizophrenia.
- Treatment Planning: Understanding your current mental state helps clinicians develop appropriate treatment recommendations. Someone with severe cognitive impairment might benefit from different interventions than someone with mood symptoms but intact cognition.
- Risk Assessment: The mental health status exam provides crucial information about safety concerns, including suicide risk, homicidal ideation, and the ability to care for oneself.
- Monitoring Progress: Serial mental health status exams allow clinicians to track changes over time and evaluate treatment effectiveness.
- Documentation: The mental health status exam creates an objective record of your mental state at specific points, which can be valuable for legal purposes, hospital admissions, or communication between providers.
What to Expect During a Mental Health Status Exam
If you’re receiving mental health care, you’ve likely undergone components of a mental health status exam, perhaps without realizing it. Most of the assessment occurs through natural conversation and observation, though some elements may involve specific questions or tasks.
The clinician may ask you to:
- Describe your mood
- Remember and recall a short list of words
- Interpret proverbs (“What does ‘people in glass houses shouldn’t throw stones’ mean?”)
- Perform simple calculations or spell a word backward
- Draw a clock face showing a specific time
These exercises help evaluate different aspects of cognition, but they’re typically woven into the conversation naturally. A skilled clinician conducts much of the mental health status exam without you even noticing.
Special Considerations in Mental Health Status Exam
Cultural Factors
Cultural background significantly influences how people express psychological distress and how clinicians interpret their observations. What might be considered unusual in one culture could be normal in another. For example:
- Eye contact norms vary widely across cultures
- Religious beliefs may be misinterpreted as delusions
- Cultural idioms of distress might be unfamiliar to clinicians from different backgrounds
Culturally competent practitioners consider these factors when conducting and interpreting mental health status exams, as outlined in the APA’s Cultural Formulation Interview.
Developmental Considerations
Mental status examinations must be adapted for different age groups:
- Children: Assessment incorporates play observation, simpler language, and age-appropriate cognitive expectations.
- Older adults: Normal age-related changes in cognition, sensory abilities, and processing speed must be distinguished from pathological processes.
Telehealth Adaptations
With the rise of virtual care, clinicians have adapted MSE techniques for telehealth settings. While this format limits certain observations (like gait or subtle movements), it offers unique windows into a person’s home environment and functioning in their natural setting.
The Future of Mental Health Status Assessment
The fundamental components of the mental status exam have remained relatively stable over decades, but technological advances are enhancing how we conduct and document these assessments:
- Digital tools now help standardize mental health status exam documentation
- Machine learning algorithms can detect subtle speech patterns associated with certain conditions
- Virtual reality environments offer standardized settings for behavioral observations
These innovations may enhance the precision of mental health status exams, though the therapeutic relationship and clinical judgment remain irreplaceable components of effective assessment.

Conclusion
The mental health status exam is far more than a clinical formality—it’s a sophisticated tool that provides a structured framework for understanding a person’s psychological functioning. While no single assessment can capture the full complexity of human experience, the mental health status exam offers valuable insights that inform compassionate, effective care.
Whether you’re a healthcare provider seeking to refine your assessment skills or someone navigating the mental health system, understanding this fundamental aspect of psychological assessment can demystify an important part of the clinical process.
For those interested in learning more about comprehensive mental health assessment, the National Institute of Mental Health offers additional resources on various assessment approaches and their applications.
Remember that while the mental health status exam provides important information, it represents just one piece of a holistic clinical picture that includes your unique history, circumstances, strengths, and challenges.
Note: If you’re experiencing a mental health crisis, please contact your local crisis line or emergency services immediately. In the US, you can text HOME to 741741 to reach the Crisis Text Line or call the National Suicide Prevention Lifeline at 988.